FRASER
HOUSE AS A PRECURSOR TO CONFEST
Qualifying as a psychiatrist in
the mid 1950s, Dr Neville Yeomans was in 1959 the founding director of Fraser
House, a psychiatric therapeutic community unit in North Ryde psychiatric
hospital in Sydney, Australia.
People who were visitors or
residents of Fraser House a therapeutic community residential unit in North
Ryde, Sydney were key folk that Dr Jim Cairns met in Paddington to plan the
first ConFest.
So who were these Fraser House
people?
Fraser house was a short-term residential
unit addressing the social basis of
mental illness and criminal behaviour. Every aspect of Fraser house
intervention was sociologically
oriented. It was based upon a social
model of mental dis-ease and a social
model of change to ease and well-being.
Residents had been transferred
to Fraser House from NSW mental homes and prisons. Yeomans observed social dysfunction as a
consistent predicative indicator of diagnosable
psychopathology and criminal
behaviour (he was at the time a government advisor on psychiatric
diagnosis). This networked
dysfunctionality among prospective patient networks was the focus of change
at Fraser House. Consistent with this, before admittance was considered, a
prospective Fraser House patient was required to attend Fraser House big and
small groups twelve times along with members of his or her family/friend
network (typically under six members), with all the network members attending
groups signing in as outpatients.
Admittance was also dependent on the network
members undertaking to continue
attending Fraser House groups as outpatients throughout a patient’s stay.
During the 1960s, Fraser House had around 13,000 outpatient visits per annum.
Fraser house patients arrived at Fraser House typically with a small (less than
six) dysfunctional family friendship network and left in twelve weeks (the
maximum stay) with a functional network of around seventy people, most of whom
lived in the same locality as the patient. Fraser house processes ensured these
expanded networks engaged in social networking and were being linked into other
Fraser House based networks in an extended network of networks.
When they arrived they had major
psychological and behavioural problems and had a dysfunctional family friend
network of five or less.
After Fraser House had been
going for around nine months residents were leaving to return to society within
12 weeks of arrival with functionality supported by a
functional family friend network of between 50 and 70 people!
Neville was looking for the best
people he could find to explore global futures and he reckoned that people with
the backgrounds these people had were ideal as they essentially had the
mainstream system knocked out of them.
The following gives some flavour
of the Fraser House processes that had such dramatic results. It also briefly
outlines psychiatrist Dr
Neville Yeomans’ (1928–2000) pioneer of psychiatric and social psychiatric
approaches in Australia.
In the 1960s and 1970s Yeomans
pioneered community psychiatry, psychiatric nursing, community mental health,
suicide/crisis telephone services, psychosocial domiciliary care, small
residential therapeutic communities and dispersed non-residential therapeutic
communities, as well as professional and peer-led psychosocial self-help
groups.

Photo - Neville and nurse at
Fraser House in 1960 (Yeomans 1965a).
A Forgotten Pioneer
Today, few people inside Australia – and
even fewer outside – may have heard of psychiatrist Neville Yeomans. In 1963,
however in an article entitled ‘the big seven secrets Australians were first to
solve’, the Sydney Sun newspaper[i]
placed Neville in a select group of pioneers and innovators which included Sir
John Eccles, winner of the 1963 Nobel prize in the physiology of medicine, and
Sir Norman Greg, nominated for the Nobel prize in physiology and medicine in
1958.
When anthropologist Margaret Mead,
co-founder (1948) and president (1956-57) of the world federation of mental
health[ii],
visited Fraser House in the early 1960s she called it ‘the most advanced unit
she had visited anywhere in the world’[iii]
and which was also praised by therapeutic community pioneer Maxwell Jones[iv].
During his career in Fraser House Yeomans
served on numerous national and international bodies[v],
which included the committee of classification of psychiatric patterns of the
National Health and Medical Research Council of Australia, the Departmental
Conference of Clinicians Panel (of which he was chairman), and the National
Foundation for the Research and Treatment of Alcoholism and Drug Dependency (of
which he was founding director).
Though largely overlooked today, Dr Neville
Yeomans’ pioneering work in Australia between 1959 and 1968 placed him then
among the internationally recognised innovators of the day, and includes him
now in the pantheon of therapeutic
community pioneers, such as Tom Main and Maxwell Jones in the United
Kingdom, and Harry Wilmer in the United States of America.[vi]
Evolving Non-Drug Based
Community Psychiatry at Fraser House
Yeomans took his first degree in biology in
the early 1950s, became a psychiatrist in the mid 1950’s, and in the early
sixties completed further studies to become a sociologist and psychologist. He
went on to become a barrister in the early seventies.
Dr Yeomans recognized that in 1957, with
considerable upheaval and questioning in the area of mental health in New South
Wales and a royal commission being mooted into past practices, there was a
small window of opportunity for innovation in the mental health area. Yeomans
had the backing of the head of the department in setting up Fraser House as an
experimental unit within the grounds of the North Ryde Psychiatric Hospital.
That Australia’s psychiatry profession was being questioned at the time is
indicated in Robson’s historical paper[vii]
on Eric Cunningham Dax’s pioneering of psychiatric change in the Australian
state of Victoria around the same time. Hinting at the state of Australia’s
psychiatric system Robson described Dax as ‘a focal point for the modernization
of a decrepit psychiatric system’. Robson quotes Ellery’s[viii]
autobiography describing Dax coming to Australia ‘to rectify the discrepancies
and supply the deficiencies of half a century’s inadequate administration of
the state’s lunacy department. Robson[ix]
also quotes Russell Pargeter, a Tasmania psychiatrist who wrote of Dax as
‘trying to reform the dreadful state of mental hospitals in Victoria at the
time’.
As founding director, Yeomans had the Fraser
House 80-bed residential unit purposely built for him by the New South Wales
Health Department during 1958-1959. Yeomans was aged thirty-one when he
obtained the go-ahead from the health department to take in male patients at
Fraser House in September 1959. The female ward opened in October 1960.
Yeomans core values included caring for and
respecting others and their functional capacities. His values framed the unit’s
evolving milieu that supported dysfunctional people turning to functional
living. Yeomans respected staff, patients, outpatients, and visitors’ capacity
to recognise and realise well being when they sense and experience it in their
lives. He wanted to explore processes with others that would recognise and use
people’s capacities for contributing to their own return to health.
The Fraser House Social system was
structured for staff and patient alike to be fully involved in evolving
transformative processes in situ. Yeomans ensured that every aspect of Fraser House was contributing to returning
residents and their social networks to functional living in society, and it
achieved that aim. Within two years the maximum length of stay was reduced to
12 weeks. Residents could return up to three times by negotiation for further
12 weeks stays.
Yeomans was looking for someone else to
research his lifework at the PhD level since the late 1960s.
Like Maxwell Jones[x]
in the UK, Yeomans evolved Fraser House as a transitional community and the
unit’s social system was designed to be tentative. Yeomans intentionally kept
these structure and processes up for continual review, change and innovation.
Sometimes a whole new set of rules and processes would be written and the old
ones dropped. Everything was in constant change and flow – staff, patients,
outpatients, processes, policies, and procedures.
Sourcing Patients and the
Fraser House Milieu
Yeomans sustained Fraser House as a balanced
community in a number of respects:
o
Half the patients at any one
time were from asylum back wards where no change was anticipated, and half were
from prisons.
o
Half were male and half were
female.
o
Half were under-active and
half were over-active.
o
Half were under-controlled
and half were over-controlled.
o
Half were under-anxious and
half were over-anxious.
Having opposites sharing the same dorm was based
on the principle that the presence of opposites creates a metaphorical normal
position in the middle. Fraser house research showed that there was indeed a
tendency towards the mean, with the under-controlled becoming more controlled,
and less active, and the over-controlled becoming less controlled and more
active.
Yeomans was quoted as saying:
We have a plan to transfer to the Centre
over a period of time all fifty Aborigines
who are now patients in NSW mental hospitals[xi].’
This happened and apart from a few that needed full time care because of
associated medical conditions, all of these people passed through Fraser House
and returned to their respective communities.
Big and Small Group Process
Yeomans set up within Fraser House a very
tight and socially ecological professional framework in which staff, patients
and outpatients together could test the potency of a specially form of caring values
based community as therapy. Contexts rich in possibilities for re-socializing
were repeated many times every weekday. Therapeutic communities in the UK and USA
had periodic whole ward meetings with up to 80 patients and thirty staff
present. In Fraser House, total community big groups (staff, patients and
outpatients attending) were held for one hour twice a day on all weekdays, with
up to 180 in attendance five days a week, all year round.
The following terms were used in referring
to the whole community meeting – ‘collective therapy’, ‘big group therapy’,
‘big meeting’, ‘big group’, ‘community meeting’, and ‘large group psychosocial
therapy’.
A Fraser House Handbook[xii]
refers to audience and crowd behaviour, especially contagion, being a central aspect of Big Group[xiii].
In Yeomans’ paper, ‘collective therapy – audience and crowd’[xiv]
he wrote:
The skilled use of collective forces is one
of the paramount functions of the socio-therapist and such skills are defined
by the team as ‘collective therapy’.
In Yeomans’ paper, ‘Sociotherapeutic
Attitudes to Institutions’ he wrote:
Collective therapy, both audience and crowd,
utilizes social forces in the patient’s primary group’.[xv]
Yeomans engaged all involved in Fraser House
(staff, patients and outpatients) in recognizing, understanding and utilizing
these social forces.
A half hour break followed Big Group where
staff reviewed the Big Group. After the half hour break, staff and attendees
were split up into many small groups where group membership was based on a
revolving set of sociological categories. The composition of small groups
varied daily. All the small groups at any one time were based on the same
category. The social categories were: age, age and sex, kinship, locality,
married/single status, and social order (manual, clerical, or
semi-professional/professional).
People in pathological social networks would
be all together with everyone else in Big Group. However, because of the
continual changing composition in small groups, the members of these
pathological networks were regularly
split up for the small group sessions. For the small groups based on
locality, Sydney was divided into a number of regions. In most cases, groups of
people came regularly on the same trains, buses and each other’s cars so they
all got to know each other. Patients and outpatients would attend the small
groups allocated by locality for their region of normal domicile. This was one
of the many aspects leading to increase in size of resident networks.
The Unit’s aim was to increase the patients’
role-taking functionality and psychological comfort. Progressively, the
patients and outpatients interaction with the Unit’s structure and process did
create more functional roles and provided ample support for residents to take
on those roles. This role-taking functionality and psychological comfort
supported their returning to functional life in their local community with an
extended and functional family/friendship/workmate network. This meant that
people who may have previously had a social network that was smaller than
typical in society, ended up having one that was typically larger in terms of
the number of people in the ‘closely known and regularly interacting’ part of
their social network.
After a time at Fraser House these
individual patient family/friendship networks would expand to have members with
cross-links to other patient’s networks, and with a continual changing Unit
population, with overlap in stays, these nested patient-networks became very
extensive. As well, all these people had Fraser House experience in common, and
a common set of mutual support skills. This networking aspect of Fraser House
was a key feature that Neville extended into the wider world. Refer:
o The All Coffee Break Conference
o UN-INMA - Atherton Tablelands INMA
Project
Governance Therapy – The Fraser
House Committee Process
Within Fraser House Yeomans pioneered
psychiatric patient committees in Australia. He set up a process whereby
patients, and their family-friendship networks as outpatients, were massively
involved in meetings and committee work – what Neville termed ‘Governance
Therapy’. Members of patients’ family friendship networks were required to
offer themselves for election to serve on committees. Fraser house patients and
outpatients progressively took on responsibility for their own democratic
self-governance. While other professionals in the UK had used patient
committees, in Fraser House the committee process was extended such that
patients and outpatients effectively became responsible for the total
administration of Fraser House.
Yeomans spoke[xvi]
of three levels of governance at Fraser House– local, regional, and global.
Every patient along with his or her respective family-friendship network was
engaged in his or her own local self-governance. The committee for
locality-based transport called the Outpatients, Relatives and Friends
Committee (one of the Fraser House committees) was engaged in ‘regional’ self-governance.
The parliamentary-pilot committees, in association with the other
sub-committees of the parliamentary committee were engaged in ‘global’
self-governance of the Fraser House ‘global commons’. The committee structure
was essentially bottom-up with committees reporting to the Parliamentary
Committee to keep this wider committee of committees informed. This three-fold
governance model involved everybody in a cross linking network of governance.
All were involved at their local level. All were involved at their regional
level. And they were all linked into global governance level process as a
serving committee person, or being engaged by, and by interfacing with the
global governance (by for example being assessed by the patient-based Patient
Assessment Committee as discussed below).
This three level (local, regional, and
global) governance at Fraser House is a micro-model of the ‘local regional
global self-governance’ model that Yeomans detailed in his paper called ‘On Global Reform’[xvii]
setting out how community psychiatry may contribute towards societal transition
to a more caring and humane world – Epochal Shift. Yeomans was not alone in
this; other people in the therapeutic community in the UK evolved models for
social reform[xviii].
However, Yeomans took the pioneering step of applying his model in systematic
sustained and prolonged action research and making this action research very
public and accessible. He also went further in evolving action research towards
global epochal transition.
Work as Therapy
It was commonly acknowledged by my
interviewees and within archival records that Fraser House psychiatric patients
and outpatients became the most skilled
in the emerging new field of community psychiatry – even ahead of the Fraser
House psychiatric staff whose prior education and training had in no way prepared
them for the Fraser House evolving milieu. Residents and Outpatients who became
experienced in community psychiatry were elected as members of the Patient
Assessment Committee. The archival material, especially the Fraser House Handbook
written by patients to train new staff[xix],
and the research interviews all support the view that Residents and Outpatients
became highly skilled in carrying out their committee and other work. In a
Fraser House Staff Handbook it was reported that patients were engaged in doing
the following work:
Perhaps the most immediate observation made
by a nurse coming to work in this therapeutic community for the first time, is
that the patients themselves have had a great deal of authority delegated to
them. Indeed, in some matters they are virtually the sole authority. At first
glance it will seem fantastic that patients assess and admit new patients;
review progress and institute treatment procedures; make new rules and alter
old ones; mete out discipline, etc.[xx]
Committees of patients prescribed community
non-drug based treatment. At first this may sound a bizarre and dangerous
notion. And yet all the reports in archival material and from interviews with
the psychiatrist, psychologists - and a senior charge nurse said the same thing
- the patients quickly emerged as the most
skilful in community therapy. According to Yeomans and the ex-staff members
Warwick Bruen, and Phil Chilmaid, none of the professional training of the
unit’s staff had in any way prepared them for engaging in community therapy.
Patients had the advantage that they
lived therapeutic community every day in the Fraser House milieu. They were immersed in it.
As an indication of the staff, patient and
outpatient competence, they effectively self-organised and ran the unit for a
number of weeks after Yeomans left for his nine month overseas trip in 1963 as
there was no replacement psychiatrist (because of no replacement being found in
time by the health department) and during these weeks things went smoothly in
the unit.
Fraser House became the centre for training
psychiatrists in community psychiatry[xxi],
with the patients as the primary source of training. Three years after the unit
started, the Australian and New Zealand College of Psychiatry co-opted Fraser
House patients as trainers of trainee psychiatrists in the new area of
community psychiatry (Yeomans, Dec, 1993, July 1998).
Linked to this patient/outpatient ‘work’ in
Fraser House governance, assessment, and therapy was the use of ‘work’ as
therapy. Progressively, patients with staff and support from other patients
took on all staff roles. The principle was ‘give the job to those who can’t do
it, with support so they learn to do it through experience’.
To provide refreshments during the break
between Big and Small Groups, the patients sought and got permission from the
North Ryde Hospital Director to set up, own, and operate their own canteen. As
another example of work as therapy, Fraser House residents tendered for a
public contract to build an outdoor bowling green in the grounds of Fraser
House. They won the tender and built the bowling green. The area is still
functional to this day – now a recreational garden. Work as therapy was also
evolving in the UK therapeutic community movement[xxii].
Fraser house pioneered home visits and
domiciliary care by psychiatric nurses and patients. A Fraser House monograph
reports that follow-up groups to homes became routine in 1962[xxiii].
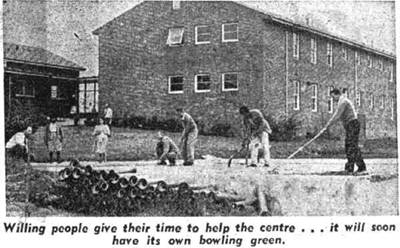
Photo two - patients building the Fraser House bowling green in the
sixties
with a dormitory in the background
(A photo from the Sydney morning herald, 11 April 1962)
Residents, who had substantially changed to
being psychosocially functional, and had been assessed as being proficient as
co-therapists, and were anticipating leaving the hospital themselves, became
involved in this Domiciliary Care process and would call on ex-residents and
their families and friends to assist and resolve difficulties[xxiv].
Fraser house, residents were helping ex-residents settle back into the
community before they became ex-residents
themselves.
Resident members of the Domiciliary Care
Committee started to go on suicide crisis calls into the community often late
at night using a red Kombi Van owned by the Residents that was purchased and
maintained by the Residents from surplus emerging from the Resident run canteen
that provide drinks and snacks after Big Group and before the following Small
Groups[xxv].
A group of patients would often go, without staff, on these domiciliary visits.
Yeomans wrote that these patients involved in domiciliary care and crisis
support were very skilled[xxvi].
Participating in domiciliary care was not time based - ‘so many months prior to
leaving’ - rather ‘psychosocial health and competency’ based.
Fraser house’s external community crisis
support service was the precursor to today’s crisis telephone line services.
The patients used red Kombi Van that the patients used for domiciliary care for
suicide crisis calls. This community-based suicide support’s precursor was
Fraser House’s ‘specialling’ process. Fraser house adopted the process of
having patients and staff constantly around potential suiciders as a support
and crisis intervention group so that suicidal people were never left alone.
This was termed ‘specialling’. Any person who was in a heightened emotional
state, disturbed or suicidal would be immediately ‘specialled’. Patients would
be co-opted as therapeutic enablers (supporting others to be able) and patients
could and did take on the role of being caring support for other patients,
especially those in danger of self-harm. Processes were set up such that a
cooperating team of patients, with or without staff, would take on the
responsibility of providing twenty-four hour support to other patients at risk
of suiciding, and in the process this support team would gain response ability.
This meant that two patients, or a patient and a staff member, would
continually stay awake with that person around the clock (and be replaced by
another shift if necessary) until, on the say so of a group, the ‘specialled’
status was removed.
Fraser house’s transforming of the
dysfunctional people at the margin of the dominant society was in the context
of Yeomans sensing that these people were the very best people to explore how
to reconstitute societies and evolve humane caring global futures[xxvii].
Everything Yeomans did in and following Fraser House was designed to fit with
everything else naturally - what Yeomans called ‘the survival of the fitting’.
Everything complemented and supported other aspects. Things that did not work
were fine-tuned or discarded. Issues that arose in one context were resolved,
or passed on to other contexts. In Fraser House, what worked (as well as
problematic aspects) was discussed with everyone in Big Group. Issues not
resolved in Big Group were passed on to small groups and vice versa. Issues
within committees were resolved, or passed on to the Parliamentary Committee.
The Pilot Committee reviewed issues within the Parliamentary Committee. Change
to functionality within three months was expected. Every aspect of Fraser House
was contributing to functionality. This pervasive inter-connected weaving of
everything with everything and connecting all of this to functionally living
together contributed to Margaret Mead describing Fraser House as the most
complete and most total therapeutic community she had ever seen, and why
Maxwell Jones said that evolution was inevitable (1969).
Yeomans set up Fraser House as a research
institute and involved the staff, patients and outpatients in the continually
studying the Unit from within. Yeomans also set up an External Research Team
focusing on Fraser House that was headed up by Dr Alfred Clark, a psychologist
from University of NSW. Additionally, Yeomans set up the Psychiatric Research
Study Group that met on the grounds of Fraser House. To this group Yeomans
attracted professionals from many disciplines. Any ideas presented at the
meetings of that group that had any relevance for Fraser House were immediately
implemented within the unit.
Yeomans maintained a very public profile for
himself and Fraser House and regularly gave public addresses about Fraser House
and wrote many press releases. Yeomans had academics and the media attend Groups
at the Unit and opened up his work and the Unit to public gaze and scrutiny
allowing the day-to-day Big Groups and Small Groups to be ‘data’ on public
display. People from religious, business, academic, non-government and
government organizations including the Federal Government Foreign Affairs
Department attended Fraser House Groups. Requests to attend were typically
granted and Fraser House became a major centre for learning group skills.
Patients and outpatients taking on functional roles during the unit’s Big and Small
Groups were on public display to these professional and lay visitors. All
visitors were signed in as Outpatients and all were fully involved. No one
attended as just an observer. Yeomans left others to draw their own theoretical
perspectives about what was happening.
Yeomans was immensely confident born of his
experience of the Unit’s functioning. When asked about ‘miracles’ at Fraser
House [xxviii]
Yeomans replied:
Of course it was miraculous. We were the best in the planet, and we all believed this, so we would acknowledge our failings, as we were streets ahead of everyone else. I was accused of being an impossible optimist. I sense i was more of a fatalistic optimist. I was context driven – if I go to ‘creative context’ then ‘everything is creative’ - it worked like that. As for the miraculous - well that was a calm night. Peaceful. Remember we were filled with the very bad and the very mad - the under controlled and the over controlled.
In 1968, Neville wrote a job description for a new role, that of NSW Director of Community Mental Health. He applied for the job and was given the job. Later he became the Founding NSW Director of Community Health as well.
It was in these roles Neville started many self-help and mutual-help groups. He worked with people in these groups to get the series of Festivals started that were precursors to ConFest.
ConFest
and the Next 250 Years