Chapter
Three – The Emergence of Therapeutic
Communities and Community Mental Health – History, Types and Significance
OVERVIEW
This chapter provides a background to my research into
Neville’s pioneering of therapeutic communities and community mental health in
THE EMERGENCE OF POPULAR/FOLK AND
SCIENTIFIC MODELS
Throughout human history there have been
popular/folk models about mental malfunction based upon culturally derived
belief systems (Engel 1977). Prior to the Twentieth Century, in the
United Kingdom, the United States of America and other places, individuals with
mental malfunctioning experienced harsh inhumane treatment (Roberts 2005a; Roberts 2005b).
Physical and mental abuse was commonplace. There was wide use of
straight jackets and heavy arm and leg iron bands and chains (Roberts 2005a; Roberts 2005b). Kennard writes of what was called as early
as 1796 ‘moral therapy’ as an early precursor to notions of therapeutic
community (2004, p. 298):
The application of therapeutic community principles to work with the chronic mentally
ill is, in many ways, the closest version of therapeutic community modality to one of its most important predecessors,
Moral Treatment. This was the term used to describe a model of care first
developed in 1796 by the Quaker William Tuke at The Retreat in York (Tuke 1813; Borthwick A., Holman C. et al. 2001).
In keeping with Quaker ideology, the mentally
ill were accorded the status of equal human beings to be treated with gentleness,
humanity and respect. This was quite revolutionary at the time, and The Retreat
also gave priority to the value of personal relationships as a healing
influence, to the importance of useful occupation, and to the quality of the
physical environment. Much of this early vision of a humane treatment for
mental illness was lost as the 19th century progressed and the mentally ill
were housed in increasingly large and impersonal asylums (Kennard 2004, p. 298).
In
What he observed was a strict non-violent,
non-medical management of mental patients came to be called ‘moral treatment’
though ‘psychological’ might be a more accurate translation of the French
‘moral’ (2005).
Notwithstanding the ‘humaneness’ of the approach, Pinel
condoned the use of threats and chains when other means failed (Dr. Grohol's Psych Central 2005).
Moral treatment was also
used by Sir William and Lady Ellis in the
1900s (History of
Occupational Therapy in Mental Health 2005) who came
to be in charge of England's county asylums. Under the Ellis’, asylums as ‘community’ had a family atmosphere and the
men and women were encouraged to enhance their previous trades or establish new
ones in order to support purposeful activity. Sir and Lady Ellis were able to
prove that the mentally ill were not dangerous with tools, and were far less
dangerous than other unoccupied individuals. The Ellis' were also responsible
for developing the idea of an ‘after care’ house, very similar to the halfway houses
of today. These places functioned as stepping-stones from total care to limited
assistance living care.
The Religious Society of Friends founded
The York Retreat and the
In the later 19th and the early 20th
centuries psychiatry was in the process of seeking links with academic
disciplines. Medicine was doing the same thing (Engel 1977; Bloom 2005). While medicine had been evolving within
biological frameworks, Rudoph Virchow writing in 1848 wrote that ‘Medicine is a
social science’ (Rosen 1974).
Bloom identifies the rise
of biopsychosocial
approaches in psychiatry in the 1920’s and traces the professional links made
by psychiatrists to evolve their specialty in the 1920s.
Bloom (2005, p.77) states:
Collaboration between
sociology and psychiatry is traced to the 1920s when, stimulated by Harry Stack
Sullivan and Adolph Meyer, the relationship was activated by common theoretical
and research interests. Immediately after World War II, this became a true
partnership, stimulated by the National Institute of Mental Health, the Group
for the Advancement of Psychiatry, and the growing influence of psychoanalytic
theory.
Bloom continues (2005, p.
81):
One piece of evidence of
this development was the emergence of the new subspecialty of social
psychiatry. Initiated in
Colloquiums were held in 1928 and 1929 under the auspices of the American Psychiatric Association Committee on Relations with the Social Sciences. As well as psychiatrists, the colloquium attendees were psychologists, political scientists, anthropologists and sociologists. These two colloquiums helped forged psychiatry’s links with the social sciences.
In the context of this reaching out to the
social sciences and as an indication of the acceptance of psychiatry by the
medical profession in the 1920’s the APA chairperson White stated during the
1929 Colloquium:
The specialty of psychiatry is almost universally
neglected by medical education (White 1929, p. 136).
Bloom (2005, p81.) quotes
Grob (1991) writing that it was,
…..the triumph of the
psychodynamic approach….that set the stage for the collaboration and
cross-fertilization of psychiatry with the behavioural and social sciences in
the 1950s.
The effects of a sociology that focused on issues of health and illness proceeded to grow in medical education, research, and the treatment of mental illness until 1980, when a distinct shift of emphasis in psychiatry occurred.
After the rise of biopsychosocial
approaches in the 1920’s there was a move away from the biopsychosocial to a
biopharmacological model in the 1980’s (Bloom
2005, p. 77):
In its role as educator of
future physicians, post-war psychiatry developed a paradigm of biopsychosocial
behaviour but, after three decades, changed to a biopharmacological model.
The definition of mental
illness as a deviant extreme in developmental and interpersonal characteristics
lost favour to nosological diagnoses of discrete or dichotomous models. Under a
variety of intellectual, socio-economic, and political pressures, psychiatry
reduced its interest in and relationship with sociology, replacing it in part
with bioethics and economics (2005, p. 77).
Speaking of the 1950-1970 period Bloom (2005, p. 82)
discusses important changes in psychiatric approach and educational method:
…the focus was on human behaviour, and the theoretic
model was psychodynamic. George Engel, in what he called the biopsychosocial
model, gave voice to this point of view more than any other single voice.
Engel and others argued for both medicine and psychiatry
to be modelled on the biopsychosocial:
To provide a basis for understanding the determinates of
disease and arriving at rational treatments and patterns of health care, a
medical model must also take into account the patient, the social context in
which he lives, and the complementary system devised by society to deal with
the disruptive effects of illness, that is the physician role and the health
care system’s. This requires a biopsychosocial model’ (1977, p. 32).
Bloom refers to Mechanic (1999) writing of the biopsychosocial being based
on a continuum and the biopharmacological being based on discrete or
dichotomous model. Mechanic describes
two definitions of mental health:
One presented a continuous model of mental health and
illness, the other a discrete or dichotomous model of mental illness. In the
first, mental health and illness are the opposite ends of a continuum; the
second rejects such a continuum, instead fitting a medical model of specific
disease categories with measurable symptoms (Bloom, 1997, p. 78).
Engel makes the point that:
Other factors may combine to sustain patienthood even in the
face of biochemical recovery. Conspicuously responsible for such discrepancies
between correction of biological abnormalities and treatment outcomes are
psychological and social variables (1977, p.132).
In the Seventies the debate about appropriate models for
both psychiatry and medicine continued. Some argued the medical model is not
relevant to the behavioural and psychological domains.
Disorders directly ascribable to brain disorder would be
taken care of by neurologists, while psychiatry as such would disappear as a
profession (Engel, 1977, p.129).
In the late 1970’s one view
of psychiatry documented by Engel was:
Psychiatry has become a
hodgepodge of unscientific opinions, assorted philosophies and schools of
thought, mixed metaphors, role diffusion, propaganda, and politicking for
‘mental health’ and other esoteric goals (Engel 1977, p. 129).
Today psychiatry has typically maintained a biopharmacological model as a biomedical sub-specialty (Bloom, 2005).
The next section explores what was actually happening to
people suffering mental malfunction since the late 1800s.
NINETEEN AND TWENTIETH CENTURY
PRACTICE
USA
In the Nineteenth Century, the
The publication by Clifford Beers of his expose of his
USA experience in the state asylum system, ‘A Mind That Found Itself’ (1908) had a wide and immediate impact both in
America and overseas towards reforming and humanizing mental health practices.
In the same year Beers founded the Connecticut Society for Mental Hygiene, and
the following year founded the
National Committee for Mental
Hygiene. This entity merged with others in the
Early Australian Experience
The Central Sydney Area
Mental Health Service’s (2004) ‘History
of Rozelle Hospital (formerly Callan Park)’ reports that:
Social deviants were often
treated brutally and alcoholism was rife in the new colony. Governor Bourke in
1820 wrote that ‘a lunatic asylum is an establishment that can no longer be
dispensed with.
The
Australian experience followed that of the
Psychiatry
in
·
1788 to
1839 - The Primitive Era. (The Beginnings)
·
1839 to 1860
- The Moral Treatment Era. (The Romantic)
·
1860 to
1945 - The Physical Treatment Era. (The Classical)
·
1945 to
the present day - The Modern Era. (The Revolution in Therapy)
On 1 July, 1876, Manning was appointed by the Colonial Government as the
Inspector of the Insane for mental institutions in NSW (The Central Sydney Area Mental Health Service 2004). Manning was noted for his humanitarianism. His
constant desire was to ensure that his patients received treatment for their
illnesses rather than confinement in a ‘cemetery for deceased intellects’.
Despite overcrowding with 1,078 patients being recorded in 1890, the
Hospital (Callan Park) at the turn of the century was considered to be one of
the ‘finest Institutions in the Commonwealth for the housing and treatment of
persons, suffering from mental disorders’ (Leong 1985).

Photo 1.
Photo of Callan Park (Leong 1985)
Two World Wars and the Great Depression brought social upheaval and
hardship and further overcrowding. Demands for financial austerity eventually
lead to
Kenmore Psychiatric Hospital
in Campbelltown which opened in January 1895 following a building
program which started in 1893 and expanded to have over 1,800 patients (Mitchell 1964).
Other large asylums were
also built in
There is no doubt in my mind that the
patients are kindly treated, and that any attempts to ill-use them would, if
they came to the knowledge of the superior officers, be most vigorously dealt
with.
Asylums in
UK
Throughout the Nineteenth
Century many madhouses and asylums were built and regulated under various Acts
of Parliament (Mind 2005). For
example, the 1828 Madhouses Act, regulated conditions in asylums including the
moral conditions. Official visitors were required to inquire about the
performance of divine service and its effects. In 1832 this Inquiry was
extended to include ‘what description of employment, amusement or recreation
(if any) is provided’.
The last of the (large)
mental hospitals to be built in England and Wales was in the early 1930’s (Roberts
2005a; Roberts 2005b).
EVOLVING THERAPEUTIC COMMUNITIES
This section discusses the
rise of therapeutic communities, the ways in which therapeutic communities
differ from asylums and the psychosocial healing potential of communal living.
Kennard refers to the link
between community and healing:
The idea of a community as a
place of healing for the troubled mind is probably universal and as old as
society itself. One of the earliest recorded intentional uses of a community in
this way was Geel in
Kennard identifies the
founding of the Little Commonwealth by
Lane was an American who had
experience as an educator at the George Junior Republic, a reformatory system
developed in the United States, and was invited to advise on the setting up of
a home for delinquent adolescents in Dorset in south west England. For 5 years
the Little Commonwealth housed around 50 youngsters, mostly aged 14–19, who
participated in a carefully structured system of shared responsibility. Lane
wrote that the chief point of
difference between the Commonwealth and other reformatories and schools is that
in the Commonwealth there are no rules and regulations except those made by the
boys and girls themselves. All those who are fourteen years of age and over are
citizens, having joint responsibility for the regulation of their lives by the
laws and judicial machinery organized and developed by themselves (Kennard 2004, p. 296).
This is an early example of the interconnected
psychosocial process of marginalized people on the fringe of society
co-constituting themselves in the process of establishing and maintaining their
lore, norms, law, self governance and shared community.
A biopsychosocial approach
addressing general health was the 1935 ‘Peckham Experiment’
at the Pioneer Health Centre in
According
to the Southwark Council Website (2005) this centre was:
…a
unique attempt to raise public health through a combination of education,
community care and preventative medicine.
The
experiment came about in response to worryingly low levels of health and
fitness amongst low-income inner-city families. Doctors Scott Williamson and
Innes Pearse (a husband and wife team) believed that social and physical
environment could have a direct affect on health - and looked to prove it.
Just
as we now join gyms, 950 families signed-up, paying one shilling a week to
relax in a club-like atmosphere where physical exercise, games, workshops and
relaxation were all encouraged. The families were constantly observed by
Williamson and Pearse's team of doctors - and attended thorough medical
examinations once a year.
The
experiment was a bold departure in the medical field in the 1930s,
concentrating on a preventative, rather than a curative approach to health -
and its setting was equally pioneering. The well-lit and open-plan design of
the building (designed by Sir Owen Williams) was far ahead of its time, providing
an ideal environment for observation and relaxation.
One
historical record describes the
large Pioneer Health Centre’s as having:
…. an out door area for roller-skating, cycling and
sports. Inside the building, you notice that large windows allow you to see the
activities of the gym, swimming pool, games area, nurseries, dance floor,
cafeteria, theatre, library and workrooms from almost any point in the
building. The facility is fully equipped with a modern laboratory and medical
staff. Many areas are designed with rollaway rooftops to allow fresh air, and
sunshine when available. The centre is designed to accommodate leisure
activities of 2,000 families (Chek 2005).
Membership of the
centre entitled all members of the family to participate in a wide range of
sports, pastimes, crafts, social and learning activities as well as community
dining.

Photo
2.
The Purpose Built Peckham Centre
- (Peckham
Health Centre 2005)
The
centre research showed significant improvement on a range of medical and
wellbeing indices compared with baseline entry levels.
The
experiment continued until 1950, concluding that: ‘It is not wages that are
lacking ... but quite simply ... social opportunities for knowledge and for
action that should be the birthright of all; space for spontaneous exercise of
young bodies, a local forum for sociability of young families, and current
opportunity for picking up knowledge as the family goes along’ (Chek 2005).
Peckham is an early example
of social learning in transitional community.
Kennard (2004, p. 304) refers to the 1939-1945 period in England
and the development of therapeutic community:
What seemed to happen at this moment in
history was that a particular constellation of human ideology, wartime
necessity, psychoanalytic insights and open mineded pragmatism came together
and coalesced into a new form of treatment.
Kennard (2004, p. 299) writes that following World War Two the zeitgeist for the mentally ill began to
change:
‘Factors which can be seen to have
contributed to this included the founding of the English National Health
Service, the emergence of sociological studies of the toxic nature of large
institutions, and the (re)discovery of a humane and egalitarian model of care
in the shape of the therapeutic community experiments during and following the
Second World War.
Bloom (2005 p.80) refers to the link between personality
and society:
The core of both social and psychiatric
theoretical speculation stimulated by the war was that the social structure and
personality are linked. Differing in its particulars but similar conceptually
was the interpretation of the hospital as a therapeutic community.
UK
The Second World War created a context that contributed
to major change in the treatment of the mentally ill. By the end of the Second
World War both
There, a group of psychoanalysts and group
therapists working with demoralized psychoneurotic ex-soldiers developed a new
pattern of institutional life (Clark, 1974, p. 29).
Weisaeth and Eitinger (1991) make the point that:
Although it is well known that the principles of forward
psychiatry were rediscovered in WWII, not everyone is aware that modern
treatment principles such as the therapeutic community and group therapy were
also developed by psychoanalysts in the British Army. The late Tom Main's ‘The
Ailment and Other Psychoanalytic Essays’ (1989) provides important information about this.
The conventional asylum of the day replicated most of the
rigid life-controlling daily routines of the returning soldiers’ former
prisoner-of-war camps. Main’s aim was to re-socialize the hospital’s patients
via ‘full participation of all its members in its daily life’.
The Northfield Experiment is an attempt to
use a hospital not as an organization run by doctors in the interests of their
own technical efficiency, but as a community with the immediate aim of full
participation of all its members in its daily life and the eventual aim of
re-socialisation of the neurotic individual for life in ordinary society (Clark 1974, p. 29; Main 1989).
Some psychiatrists caring for these ex-soldiers
recognised that major changes to ‘treatment’ had to occur for these people to ever
be able to return to functional living in society. Psychiatrists began
exploring community-based approaches to reconnect these former soldiers with
society. Given the community approaches being used, these units became known as
therapeutic communities.
Maxwell Jones is recognized as the main developer of
therapeutic community (Jones 1953; Jones 1957). In contrast to the conventional
asylums, Jones writes of starting at
By great good fortune I was asked to organize
a treatment unit for British ex-prisoners of war who had just returned from the
prison camps in
And so, almost imperceptibly we moved from
the idea of teaching with a passive, captive audience, to one of social
learning as a process of interaction between staff and patients. By the end of
the war we were convinced that people living together in hospital, whether
patients or staff, derived great benefit from examining, in daily community
meetings, what they were doing and why they were doing it (Jones 1968, p. 16-17).
Kennard writes of wide interest in Jones’ work (2004, p. 299):
Right from its early days
Maxwell Jones’ experiment at
In stark contrast to conventional asylum top-down
autocratic structure, Maxwell Jones writes of re-constituting towards democratic
egalitarian structure/processes having three main objectives – communication,
decision-making and culture:
…the establishment of two-way communication
involving as far as possible all personnel, both patients and staff; decision
making machinery at all levels, so that everyone has the feeling that he is
identified with the aims of the hospital, with change, and with its success and
failures; the development of a therapeutic culture reflecting the attitudes and
beliefs of patients and staff and highlighting the importance of roles and role
relationships (Jones 1968, p. Xlll).
These changes in communicating, decision-making and
culture were core shifts in changing from top-down expert driven hierarchy to a
democratic egalitarian holarchy (each participant as networked part of the
whole) with a community focused structure:
In a therapeutic community communications at
all levels are made as efficient as possible, and decision-making by consensus
is aimed at.
In a therapeutic community, a unilateral
decision, no matter how wise, is seen as contradictory to the basic philosophy (Jones 1969, p. 48).
In this shift to a flatter structure, Jones suggests that
a more apt name for the leader is ‘catalyst or charismatic leader’ (Jones 1969, p. 24).
Two-way communication and all-inclusive meetings change
the notion of ‘confidentiality’. Information is to be kept confidential within
the community, not just within the patient-psychiatrist relationship (Jones 1969, p. 54).
In his book ‘Administrative Therapy’, D, H. Clark (1964) writes of using meetings and other aspects
of administration as an integral aspect of patient change, what he called
‘Administrative Therapy’.
Maxwell Jones expands on these re-socializing themes:
The psychiatric hospital can be seen as a
microcosm of society outside, and its social structure and culture can be
changed with relative ease, compared to the outside. For this reason
‘therapeutic communities’ to date have been largely confined to psychiatric
institutions. They represent a useful pilot run preliminary to the much more
difficult task of trying to establish a therapeutic community for psychiatric
purposes in society at large (Jones 1968, p. 86).
In a conversation I had with
Alfred Clark (June 2004) he recalled the term ‘civil
reconnection’ for what the
Jones saw therapeutic community as an adjunct to existing
processes:
It does not amount to a treatment methodology
in its own right but complements other recognized psychotherapeutic and
pharma-cological treatment procedures (1969, p. 86).
Jones and others recognized potential in hospital social
restructuring:
A hospital has the advantage of being a small
community where it is possible to organize the social structure so that it
enhances social learning (1969, p.91).
Jones called this setting up a ‘living-learning’
situation:
The term is meant to convey the concept of
social learning as it applies to the problems of everyday living (1969, p. 87; Kennard 2004).
Jones adds that along with structure - roles, role
relationships and culture may be involved in re-socialising:
The concept of the therapeutic community
stresses the importance of social structure; it underlines the need to focus on
roles and role relationships and to evolve a therapeutic culture (1969, p. 86).
David Clark, in writing the history of
…mixed-sex wards, no staff uniforms, ward
meetings, staff discussion groups and open and free discussion between
professions. There was plenty of encouragement for patients to help each other
and to talk openly with staff, as well as active involvement of, and discussion
with relatives of patients (1996).
Other aspects were:
Doctors’ Sensitivity Meeting on Fridays (with
its egalitarian sharing), the Hospital Innovation Project, and the culture of
growth.
Basic premises of the therapeutic community
are the abolition of hierarchy and authority, the establishment of all
contributions as equally valid, the tolerance of open confrontation and
challenge, and the acknowledgement of patients’ responsibility for their own
lives and for the running of their wards (1996).
Patients became change-agents of self and others.
Patients also became community leaders.
The task of senior officers like myself, the
power holders in the organisation, was supportive – creating an atmosphere
where hope could develop.
It taught us to value the contributions of all the people
who worked with patients and showed us the immense power of social forces in
the life of the ward (Clark 1996).
David Clark writes of Maxwell Jones:
Jones himself said that the distinctive
aspect of the method was ‘the way the institution’s total resources, both staff
and patients, are self-consciously pooled in furthering treatment (1974, p. 29).
Jones contrasts therapeutic community with conventional
treatment.
In therapeutic communities - active rehabilitation,
democratisation, permissiveness and communalism replace the conventional
custodialism and segregation, old hierarchies and status differentiation,
customarily limited ideas and the specialized role of the doctor (1968, p. 87).
Jones refers to meetings playing a central role:
An essential feature of the organization of a
therapeutic community is the daily community meeting. By a community meeting,
we mean a meeting of the entire patient and staff population of a particular
unit or section. We have found it practicable to hold meetings of this kind
with as many as 80 patients and up to 30 staff; we think that the upper limit
for the establishment of a therapeutic community in the sense that the term is
used here is around 100 patients…it is desirable for the community meetings to
be followed by meetings of these smaller groups (1968, p. 87-88).
David Clark writes of
The centre of Belmont Life was the morning
meeting, attended by all members of the community, where all matters of general
interest were analysed. There was a system of feedback of the events of the 24
hours. This was followed, always, by a staff review session, where the main
meeting was analysed and personal contributions and reactions assessed (1974, p. 30).
Rather than been seen as a negative, crisis situations
were used to foster change:
The social organization inherent in
therapeutic community settings – both inside and outside the hospital -
strongly facilitates the productive resolution of crisis situations by
confrontation (Jones 1969, p.86).
The therapeutic
community process was largely responsible for the return of war neurosis
soldiers to mainstream society. According to Jones, at
…the group that benefited most
from the therapeutic communities were the patients (and staff) trapped in
long-stay wards. By 1980 most of those patients had left hospital (1996).
USA
Kennard (2004) refers to the writing of Boston psychiatrist
Bockoven (1956) who described ‘the heavy atmosphere of
hundreds of people doing nothing and showing interest in nothing’ in American
hospital wards in the1950s.
Sandra Bloom (1997) refers to the U.S.A. development of
therapeutic community having similarities to the UK treatment of war neurosis.
During the same
era in the
SOCIAL PSYCHIATRY, SOCIAL THERAPY AND MILIEU THERAPY
This section details some of the terms and processes
associated with therapeutic communities.
Jones defines social psychiatry as:
The preventative and curative measures, which
are directed towards the fitting of the individual for a satisfactory and
useful life in terms of his own environment (1968, p. 29).
Jones further writes on social psychiatry:
Sociocultural process is an integral part of
the treatment. The sort of social system that results is often called a
‘therapeutic community’, or in terms of social process, milieu therapy.
What distinguishes a therapeutic community
from other comparable treatment centres is the way in which the institutions
total resources, staff, patients, and their relatives, are self consciously
pooled in furthering treatment. This implies above all, a change in the usual
status of patients. In collaboration with staff, they now become active
participants in their own therapy and that of other patients and in many
aspects of the unit’s general activities. This is in marked contrast to their
relatively more passive, recipient role in conventional treatment regimes (1968, p. 85-86).
Kennard describes distinguishing features of
therapeutic communities as:
There is a ‘culture of
enquiry’, a phrase that highlights the need not only for efficient structures
but for a basic culture among the staff of ‘honest enquiry into difficulty’,
and a conscious effort to identify and challenge dogmatic assertions or
accepted wisdoms.
The basic mechanism of change can be described as this:
the therapeutic community provides
a wide range of life-like situations in which the difficulties a member has
experienced in their relations with others outside are re-experienced and
re-enacted, with regular
opportunities - in groups, community
meetings, everyday relationships
and, in some communities, individual psychotherapy - to examine and learn from
these difficulties. The daily life of the therapeutic community provides opportunities to
try out new learning about ways of dealing with difficulties (2004, p. 2).
In the context of therapeutic communities, David Clark (1974, p. 14) defines ‘social therapy’ (a term linked to
therapeutic communities) as:
… an attempt to help people to change by
affecting the way in which they live.
This is based on the observation that:
…people are shaped by the way they live,
unfortunately often for the worse (Clark 1974, p. 14).
Carstairs in the Forward to David Clark’s book quotes
another of
…the use of social and organizational means
to produce desired changes in people (Clark 1974, p. 8).
Carstairs also quotes David Clark’s third definition:
Social therapy is about personal change and
growth and living-learning experience (Clark 1974, p. 8).
David Clark suggested that social therapy could be
summarized using three words – ‘Activity’, ‘Freedom’ and ‘Responsibility’.
Jones notes the ‘experience of two centuries’ of the corroding effect of
idleness. A central focus was the potential of a community exploring freedom
and responsibility together (1974, p. 67).
The common theme through the above summary of therapeutic
community experience has been the use of social processes, especially community
meetings, as the change process. Chapters Six to Ten will detail how Neville
went way beyond the above in Fraser House.
The next section explores the intervening forces
contributing to a decline in the use of therapeutic communities within
psychiatry.
DECLINE OF THERAPEUTIC COMMITTEES
IN THE UK
David Clark, in Chapter Eight of his book ‘The Story of a
Mental Hospital: Fulbourn, 1858-1983’ (1996), details the reasons for the decline of
therapeutic committees in the UK National Health system.
In 1970, four
wards in Fulbourn hospital had been therapeutic communities and a number of
hospitals had therapeutic communities. David Clark writes of the
During the 1960s therapeutic communities had started in
many psychiatric hospitals; Henderson, Claybury, Littlemore, Fulbourn,
Dingleton and Ingrebourne became well known. In the 1980s therapeutic community
wards stopped operating, units were closed, hospitals famous for being
committed to therapeutic community principles, such as Claybury, dwindled in
size and ultimately were being closed down (1996).
The root cause is the incompatibility of an
egalitarian, democratic ward culture with the authoritarian, bureaucratic
organisation which the National Health Service has gradually become.
… the hostility of powerful senior doctors to
a system that devalued their expertise and challenged their power worked
against it, and the National Health Service Bureaucracy of the 1990s, with its
emphasis on ‘business management’, strict economy, and answerability upward
could not tolerate a system so challenging, so revolutionary and so irregular.
Enthusiasm and hope do not appear in accounting
systems.
The external response was as suspected; David Clark
writes:
A unit where patients make decisions, where
disorder is apparent and from which unacceptable demands may come, perplexes
and angers tidy-minded and harassed managers so that they readily support
demands for enquiries, disciplinary action and closure (1996).
Clark (1996) describes the
British psychiatry has moved away from an interest in
social therapy. With a wider range of new drugs available, many young
psychiatrists concentrate on improving their skill in diagnosing, assessing
symptoms, prescribing drugs and monitoring side effects.
The insecure and inadequate doctor feels far safer in a
white coat examining a half-naked patient with a stethoscope or in a
comfortable armchair out of sight behind the psychoanalytic couch, than working
in an environment where he would be open to scrutiny and criticism by patients
and nursing staff.
Clark (1996) also writes about the Nation Health Service
funding in the Seventies and Eighties:
Most of their time and energy was given to
general hospitals which had a clear traditional social structure of doctors
doing their skilled work, nurses assisting and organizing, and patients lying
passively in bed awaiting cure.
The National Health Service, David Clark writes, is now:
…where power and authority is statutorily
entrenched with administrators, consultant doctors and senior nurses and where
patients are usually treated as passive, incompetent, ignorant people whose
only task is to await the attention, skill and compassion of those paid to look
after them (1996).
Clark (1996) details
some of the lasting effects of the therapeutic community movement in the UK:
Quite a few of the practices of the
therapeutic community were by now accepted as normal in Fulbourn - mixed-sex
wards, no staff uniforms, ward meetings, staff discussion groups and open and
free discussion between professions.
Is any of what we learned
and taught still relevant? I believe most of it is. Some of the effects of the
social revolution in post-war British psychiatry remain and will I believe be
permanent. Psychiatric nurses today see their main tasks as listening to patients,
counselling them and understanding them. They know they do this best in a
supportive, friendly humane culture. Most British psychiatric wards and units
are now open door. In many units nurses, patients, and creative therapists meet
in groups and in ward meetings. This is a far cry from the psychiatric nursing
culture of the forties with its emphasis on order, uniforms, discipline and its
undertone of brutal oppression.
DECLINE OF THERAPEUTIC COMMITTEES
IN THE USA
Commencing in 1968, Paul and Lentz (1977) set up the first research in USA on long
term chronic mental patients - comparing two psychosocial change programs with
a comparison hospital treatment. One of their change programs was based on
milieu therapy (or therapeutic community) and the other on social learning
(using a token economy). 92% of the patients in the social learning program
were released with community stay without rehospitalisation for the minimum
follow up period of 18 months.
After four and a half
years of results demonstrating that the two psychosocial programs were clearly
superior to the comparison hospital, they were going to move the hospitalised
‘patients’ into the social-learning unit. However, before they could do so,
medico-political forces shut both of the psychosocial change programs down and
ended the research. Shortly afterwards, interests holding to the
biopharmacological model linked with forces within the politico-legal system to
get laws passed prohibiting many of the key aspects of the psychosocial change
programs. The effect of these laws and regulations were that aspects of
therapeutic community based programs that Paul and Lentz’s research had
empirically demonstrated as possessing considerable change power were banned.
These changes to the law left the least
useful and most expensive treatment,
namely drug-based long-term hospitalisation as the only option remaining for
long term chronic mental patients still in the hospitals. The ‘patients in and
none out’ process would ensure that this pool of patients would steadily
accumulate in the back wards.
Kennard (2004, p. 302), in referring to the success of the Soteria
House Therapeutic Community Experiment, which found the Soteria program was as
effective as neuroleptics in reducing the acute symptoms of psychosis, writes:
Surprisingly, the
success of this experiment has not spawned a host of replicas, pointing up the
conservatism of the professional establishment, the reluctance to use the
natural healing properties of normal relationships, and the hold that the drug
industry still has over treatment models.
WIDER APPLICATIONS OF THERAPEUTIC COMMUNITY
In reviewing the various
settings for therapeutic community Kennard introduces the term ‘therapeutic
community impulse’ as:
….something that flows through many forms of
institutional care, including hospitals, schools, prisons and other settings
created by societies for their ill, disabled or troublesome members (and
sometimes for their brightest too). This impulse comprises a tolerance of the
expression of conflict, a desire to enable people to take responsibility for
their lives, a natural sense of democracy (not necessarily of the one vote per
person variety) where everyone has the right to information and to contribute
to decisions that affect them, and ‘a kind of shirt-sleeves informality about
the business of helping people.’ I believe it is a hardy plant because once
experienced, the capacity to work with people in this way becomes an inner
benchmark of the most humane and effective way of delivering mental health care
(1998, p. 27).
Kennard (2004) reviews the application of therapeutic community as an adaptable
treatment modality across different settings in UK, USA, in Africa and in 11
out of 15 European Union countries – including youth offenders, drug addicts,
and within prisons. Kennard refers to Kasinski’s review of the use of
Therapeutic Communities for Young People as ‘Planned Environment Therapy’ (Kasinski 2003; 2004, p. 297).
In discussing therapeutic
communities in prison, Kennard writes (2004, p. 302):
Prison may seem an unlikely
setting for a treatment model based on democratic decision-making. Yet democratic therapeutic communities have been run in prisons since
the 1960s with positive results, and today there is an increasing number within
the English prison system. The first and best known of these is Grendon Prison,
30 miles west of London, which
opened in 1962 and takes long-term male prisoners towards the end of their
sentence. Violence, sex offences and robbery are the most common types of
offence.
Once accepted, a prisoner moves to one of
five wings of 40 men, each run as a separate therapeutic community, where he
may stay for up to two years.
In Grendon:
…considerable thought is given to how the key
therapeutic principles can be adapted (Cullen 1997; Kennard 2004, p. 303).
Neville spoke to me (Dec
1993, Sept 1998) about Grendon Prison (Association of Therapeutic Communities 1999; Smartt
2001; HM Prison Grendon 2005) in the UK. Grendon has had excellent
recidivism rates (Millard 1993; HM Prison Grendon 2005) - way ahead of traditional maximum security
prisons - for over thirty years. Cullen (1997) reports the overall recidivism rate for men
who have served some time at Grendon being 33%, and for those completing their
program it falls to 16% compared with a 42 to 45% recidivism rate for the
national rate. An article in the
Birmingham Post newspaper states:
Grendon is the
only prison in Britain that operates wholly as a therapeutic community; it has
a waiting list of around 200 prisoners who want to go there and, uniquely,
independent research has just shown that prisoner who complete its therapeutic
regime are significantly less likely to re-offend when released (A Prison to Cure and Not to Punish 1998).
On therapeutic communities applications within the
criminal justice system Kennard concludes:
In the experience of the
author and other experienced practitioners in both the USA (Toch 1980) and
Europe (Cullen and Woodward 1997) therapeutic communities in prisons can be surprisingly
effective in creating a culture of openness and exploration of personal issues,
in direct contrast to the conventional prison culture, and also in reducing the
incidence of violent disturbances. Perhaps the major limitation is the acceptability
of the model to prison staff and administrators. For some staff the relaxation
of the “them and us” polarisation of officers and inmates provides a welcome
opportunity to do something worthwhile; for others it is seen as a threat to
their authority and control (2004, p. 303).
Paul Hamilton (1992) describes a therapeutic community
in K Division in Pentridge Prison in Melbourne, Australia as:
… having a valuable catalytic effect
in terms of education and work practices, as well as providing a relatively
normal environment for HIV seropositive prisoners.
Within
Many therapeutic community Drug and
Alcohol Rehabilitation Centres in
1.
Residents
participate in the management and operation of the community
2.
The
community through self-help and mutual support is the principle means of
promoting behavioural change
3.
There
is a focus on social, psychological and behavioural dimensions of substance
abuse (Gowing, Cooke et al. 2005)
The next section describes ways in which therapeutic
community processes were extended into the wider community.
REHABILITATION SERVICES,
TRANSITIONAL FACILITIES AND THE MOVE TO COMMUNITY BASED CARE
David Clark writes of the setting up at Fulbourn Hospital
of Rehabilitation Services starting in the 1970s and fully developed during the
1980s, as being another aspect of social therapy. These Rehabilitation services
were precursors to Community Mental Health.
We had moved most of our long-term patients
out of hospital into group homes, halfway houses, sheltered accommodation and
so on. We were visiting and supporting them there. We had developed an
effective system of care in the community - long before it became official
government policy.
Many hospitals emptied the wards too quickly,
with inadequate support facilities. We took longer over the process. We set up
a wider range of transitional facilities. We prepared people carefully for
discharge. We supported them in the community. We certainly had remarkably few
episodes of suicide, social breakdown or public disaster over the years while
we were opening the doors.
We developed
transitional facilities, halfway houses, group homes, sheltered accommodation.
We set up sheltered workshops and industrial units and organised supportive
rehabilitation using networks of social workers, community psychiatric nurses
and community occupational therapists, and so on (1996).
Kennard writes of the
application of therapeutic community practices to patients in community based
transitional facilities who were no longer ill or could now have their symptoms
controlled by the newer medications, and whose continued hospitalisation was
due at least partly to a loss of the skills and confidence to manage their own
lives.
As these patients left
hospital, those who remained
were those whom today are sometimes referred to as the ‘difficult to place’,
whose combination of treatment resistant symptoms and difficult personalities
keep them in need of 24-hour care. Thus although the crusading aspect of the therapeutic community approach to chronic mental illness is
relevant where total institutions are still found, today there are other
important applications in community-based housing projects for the long term
mentally ill, and the work of community
mental health teams. Small
domestic households of between 5 and 12 residents live with staff support
(either 24 hour or office hours depending on the level of need). For people
with more integrated or recovered psychoses there are regular community meetings, service users help to draw up and review their
own care plans and those of their fellow residents, and help in running the
household (2004, p. 303).
COMMUNITY MENTAL HEALTH - THE UK ,
USA
This section outlines the
…an appropriate
perspective for all community-based services. The emphasis on respect for the
individual, the recognition that services users have therapeutic skills, the
importance of a containing environment and awareness of the potential for
splitting within teams and organizations have been noted as some of the
contributions that the therapeutic community approach can make to the work of
community mental health teams (Kennard 2004, p. 300)
United States
Community Mental Health was promoted in the United States
as a new wave of ‘expanded mental health care’ (Citizens Commission on Human Rights 2005).’
Given this aspiration, the organisation LA Voice writes:
There's no question that deinstitutionalising the
mentally ill ended (for the most part) the cuckoo's-nest
horrors of 1950-60s mental hospitals. But it also consigned people with
a horribly difficult-to-manage, stigma-ridden lifetime illness to a ragged net
of jails, outpatient programs and halfway houses from which the Legislature
often enjoys siphoning money. End result? People get dumped back onto the
street.
The Times points out that 34% of the 83,347 homeless in
greater L.A. are severely mentally ill; 47% of the total are chronic substance
abusers and 19% are veterans (though it doesn't say how much those three
numbers intersect) (LA Voice 2005).
Given the concerns, across
each State in the
Mediation has been evolved in some parts of the world as
a way of settling issues in dysfunctional families (Carlson 1971). One such example is the Ontario Family
Mediation Centre (2005), which was highly regarded by Neville (July
1998).
Community Mental Health in the UK
Clark (1996) writes that as a result of the social revolution in
post-war psychiatry in the UK, the care of people with long-term mental disability
has been changed utterly:
Very few of them are now in hospital wards.
Many live in the community, with their families or in sheltered accommodation.
They attend day centres and workshops and are supported by teams of social
workers and community nurses. We have created in
The 4 November 1999,
BBC program ’Background Briefings’ spoke of care in the community representing ‘the biggest political
change in mental healthcare in the history of the NHS.
It was the
result both of social changes and political expediency and a movement away from
the isolation of the mentally ill in old Victorian asylums towards their
integration into the community. The aim was to ‘normalise’ the mentally ill and
to remove the stigma of a condition that is said to afflict one in four of the
British population at some time in their lives.
The main
push towards community care as we know it today came in the 1950s and 1960s, an
era which saw a sea change in attitude towards the treatment of the mentally
ill and a rise in the patients' rights movement, tied to civil rights
campaigns.
The 1959
Mental Health Act abolished the distinction between psychiatric and other
hospitals and encouraged the development of community care (BBC News
2005).
An Internet source document from the UK NGO
‘Mind’, formerly ‘The National Association for Mental Health’ entitled ‘Key
Dates in the History of Mental Health and Community Care states:
From 1955
onwards, psychiatric in-patient numbers began to slowly decrease due to the introduction
of social methods of rehabilitation and resettlement in the community, and the
availability of welfare benefits, as well as the introduction of antipsychotic
medication (Mind 2005).
The same ‘Key Dates’
document identifies 1961 as the
year Enoch Powell, as Health Minister, made his famous ‘Water Tower’ speech to
the Annual Conference of the NGO Mind.
He envisaged that psychiatric hospitals would
be phased out and care provided in the community. Powell’s plan was for
‘nothing less than the elimination of by far the greater part of this country’s
mental hospitals as they stand today’ (2005).
The ‘Key Dates’ document refers to:
The Hospital Plan for
In-patient numbers continued to fall, but
many local services were not yet in place. A new group of ‘long-stay’ patients
began to accumulate in the hospitals. The era of community care had begun and
this has remained official policy ever since (2005).
Sir Roy Griffiths’ 1988 UK report, ‘Community Care:
Agenda for Action’ was a precursor to the Community Care Act of 1990, that set
up community care as it has operated through the Nineties
(Mind 2005).
In 1998 in the
Care in the community has failed. Discharging people from
institutions has brought benefits to some. But it has left many vulnerable
patients to try and cope on their own. Others have been left to become a danger
to themselves and a nuisance to others. A small but significant minority have
become a danger to the public as well as themselves (Mind 2005).
Burns and Priebe (1999, p.
191-192)
outline issues in Mental Health Care in the UK:
The past few years have seen mental health
services in
We’re mad to trust shrinks – Daily Mirror, 9
February 1996.
The current, pervasive
opinion is that English mental health services (especially in cities) are
unacceptably poor (Deahl and
Turner 1997).
Burns and Priebe (1999, p.
191-192)
also refer to comments by Frank Dobson (1990):
The Secretary of State for
health, Frank Dobson, has recently pronounced that ‘community care has failed’,
and his predecessors expressed their lack of confidence by imposing a succession
of increasingly restrictive legislative requirements – the Care Programme
Approach.
Burns and Priebe detail
shortcomings:
There are undoubtedly
serious short-comings in the English services. These include the excessive
preoccupation with risk, the limited therapeutic involvement of consultants and
the shortage of services for patients with less severe mental illnesses, to
name just a few (1999).
In the same article Burns
and Priebe also comment on considerations of clinical effectiveness:
Service delivery is
generally transparent and subject to clinical audit and a widespread
consideration of clinical effectiveness. English psychiatrists, correctly
preoccupied with the problems generated by the split between health and social
care, seem rarely to reflect on the degree to which services are fragmented elsewhere.
By international standards our services are extraordinarily straightforward and
well co-ordinated (1999).
They also provide the
following contextual information:
Neither one of us doubts the
real problems that face modern mental health services. The rules of the game
are changing. Family and social changes make coping with severe mental illness
increasingly problematic. Public expectations are rising, and in our current,
very visible position, balancing therapy with social control is highly
delicate.
There is no shortage of
advice about how to reform the mental health services being proffered by
pressure groups and voluntary bodies. In many cases their conviction may far
exceed evidence for the feasibility or value of their proposals (1999).
Community Mental Health in Australia
Community Mental Health in
As one indicator of the current status of
community mental health care the Weekend Australian newspaper 16 July 2005 ran
a headline ‘Time to Get Mentally Ill Out of Jails’:
Leading psychiatrists have admitted that a
twenty-year policy of treating mentally ill patients in the community has
failed. The psychiatrists are demanding radical review of mental health care
claiming prisons have replaced asylums as holding centres for the mentally ill.
Those calling for a new approach include many of the architects of the current
policy of de-institutionalisation, which lead to the closure of psychiatric
wards and institutions around the country.
A recent study by the Corrections service
found that 74% of prisoners in NSW suffer from a psychiatric disorder with
almost 10% suffering symptoms of psychosis (Kearney and Cresswell 2005).
SELF-HELP AND MUTUAL AID GROUPS
Another development in the
1960’s was psychosocial self-help/mutual aid groups where people with mental
malfunction provide each other mutual support without the presence of mental
health professionals. Historically, governments and their agencies, as well as
private service providers, have provided care to the mentally disabled as a
funded service. After self-help and mutual aid processes were evolved in
therapeutic communities, ex-patients of these communities began forming their
own self-help groups in civil society. This led to the growth of voluntary
not-for-profit psychosocial self-help group movement in the
Kyrouz,
and Humphreys (1997) carried out a review of research carried out in the 1980s
and 1990s on the effectiveness of self-help mutual aid groups. Their review
primarily covered studies that compared self-help participants to
non-participants, and/or gathered information on multiple occasions over time
(that is, “longitudinal” studies).
They summarise findings of five research studies on
mental health groups as well as research on self help groups focusing on
suffers of bereavement, diabetes,
cancer, chronic illnesses as well studies on self-help group for caregivers as
well as groups for elderly people.
Kyrouz, and Humphreys (1997) report:
Most research studies of self-help groups have found
important benefits of participation.
ORGANIZATIONS,
NETWORKS AND MUTUAL HELP PROVIDING SUPPORT AND SUSTENANCE TO MARGINAL PEOPLE
Healthy Living Centres
Influenced
by the Peckham Experiment mentioned previously, the
Its
aim is to improve health through community action and particularly
to reduce inequalities in health in deprived areas.
Healthy living centres will
take various forms and may exist as partnerships and networks rather than as
new buildings. They are based on a recognition that determinants of
poor health in deprived areas include economic, social, and
environmental factors which are outside the influence of
conventional health services (BMJ
Editorial 1999).
Everyday Life Mutual Help
Rowan Ireland (1998),
a Melbourne sociologist had been researching an urban renewal social movement
among the extreme poor in São Paulo, Brazil in the late eighties.
Ireland refers to Evers' (1985) writings
on new social movements in Latin America. Like
Natural Nurturers in Everyday Life
Resonant with the São Paulo
experience above, a report of a visit (where I was a member of a international
team) to the Southern Philippines war zone of Pikit, Mindanao identifies
‘natural nurturer networks’ among the local rice farms living in the war zone
as an integral aspect of ongoing social support among local people:
Given the limitations and
the short period allotted, the team achieved the objectives of the pre-test,
especially in drawing out local contexts, identifying local healing ways, and
natural nurturers says international team member and UP CIDS PST research
fellow, Faye Balanon. More importantly, there is the need to help identify
local psychosocial support systems, especially in the areas struck by
calamities, and to identify people in the local cultural context – the natural
nurturers who could support the psychosocial needs of the community after the
team has left (Balanon
2004).
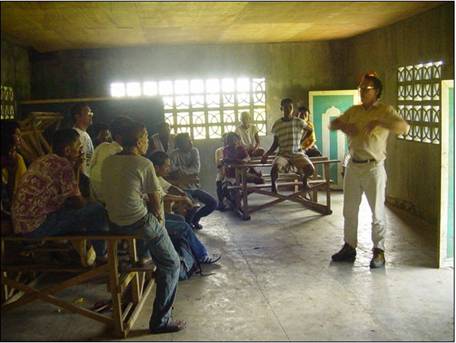
Photo
3
Engaging with Muslim Men’s Group in Pikit Area – used with permission
Chapters Twelve and Thirteen extend this theme of natural
nurturers.
POSSIBLE FUTURES
As in the call to recreate the old asylum culture in Australia
(Kearney
and Cresswell 2005), the same trend is emerging in the UK.
A malignant
trend in English society in the 1990s is the growth in the number of gaols and
secure institutions.
Wherever society locks up people it dislikes and pays other people to
keep them in, an oppressive and cruel culture is likely to develop. If
society designates these prisoners ‘insane’ and hires doctors and nurses as
gaolers, they will create the same medicalised, hypocritical gaol culture as in
the old asylums (1996).
SHIFTS IN PSYCHIATRIC MODELS
This section returns to the
theme of psychiatric models and explores forces influencing them in the past
few years. Burns and Priebe (1999, p. 191-192) writing of the UK psychiatric experience
point out the players involved in the underlying economics and review of
effectiveness of mental health service provision:
Mental
health care is, with few exceptions, within the public domain, and service
planning is not solely driven by the economic interests of service providers
and insurance companies.
The powerful forces
associated with psychiatric paradigm shift mentioned at the beginning of this
chapter are currently being confronted by Victorian Workcover, a State body in
The five core principles reflect contemporary practice
in injury management and focus on:
1.
a demonstration of measurable
treatment effectiveness
2.
a biopsychosocial approach for the
management of pain
3.
empowering workers to manage their
injury
4.
treatment goals that focus on
function and return to work and
5.
the delivery of treatment based on
the best available evidence.
With respect to the
‘psychosocial’ component of biopsychosocial,
the terms ‘functional
overlay’, ‘somatoform reactions’ or ‘psychosomatic reactions’ are used when
people have a psychological overlay suppressing or inhibiting
physiological function. Typically, Workcover claimants with functional overlay
are referred to a psychiatrist or psychologist. Rather than the previous norm
of expert based assessment, the clinical framework requires the use of
standardised outcomes assessment of:
1.
Physical
impairment
2.
Activity
limitations
3.
Life
participation restrictions
‘Life participation
restrictions’ asks for considerations on a wellness continuum rather than
nosological diagnoses of discrete or dichotomous conditions.
For psychiatrists and other
caregivers to continue to receive funding for their Workcover claimants, they
need to demonstrate measurable treatment effectiveness
resulting in the enhancement of at
least two of the above three domains. Independent standardised outcome
assessment has to be used. There is also a provision that the treatment must
focus on empowering the claimants to manage their own injury. Another provision
is that treatment goals must be functional and focused on a return to work.
It is understood that the Transport Accident Commission is likely to introduce
a similar Clinical Framework. This
outside intrusion into the power domain of psychiatrists, psychologists, and
other professionals is being strongly resisted by them (from discussion at an
Australian Wellness Association Forum in
Having a ‘return to work’
focus is isomorphic with a concern to have people returning to functional
living in society rather than being warehoused in asylum back wards like
soldiers with war neuroses. The Clinical Framework does hold a space for a
psychopharmacological approach; drugs may be an aspect of treatment. The
framework changes the patients’ role from being a passive and dependent upon a
professional expert to having an active self-help role with a functional return
to work focus. The potential role of Neville’s biopsychosocial processes in the
context of the Workcover Clinical Framework is discussed in Chapter Ten, Eleven and Thirteen.
THE PSYCHOSOCIAL MODEL, THERAPEUTIC
GOVERNANCE AND
GLOBAL SOCIAL CONTROL
Vanessa Pupavac (2005) in her paper ‘’Therapeutic Governance: the Politics of Psychosocial
Intervention and Trauma Risk Management’ argues the international psychosocial model and its
origins in an Anglo-American therapeutic ethos is being used for social control
via pathologising of Third and Fourth World countries by wide interests in the
First World. Her paper argues that
‘psychosocial approaches jeopardise local coping strategies’ and identifies ‘the potential political, social and psychological
consequences of the pathologisation of war-affected societies’. Her paper
concludes ‘that therapeutic governance represents the reduction of
politics to administration’. Pupavac argues that powerful first world entities
assume pervasive pathology exists in third and fourth world societies and take
action that strengthens that assumption, and then uses the claimed pathology to
take on a ‘therapeutic governance’ role on behalf of ‘helpless’ people.
Power is not exercised by the ostensible subjects
of rights, but by international advocates on their behalf.
Effectively, the psychosocial model involves
both invalidation of the population’s psychological responses and their
invalidation as political actors, while validating the role of external actors.
Where populations are experiencing a
curtailment of self-determination and a questioning of their moral capacity, it
should be no surprise if psychosocial professionals find a relatively high
instance of depression - the link between a sense of control and mental health
is well established. However, the presence of depression does not vindicate
therapeutic governance, rather the reverse. It is the functionalism of
therapeutic governance that needs to be examined. Ironically, the unprecedented
regulation of people’s lives and emotions under therapeutic governance risks
populations’ mental health. That populations do not succumb to the
pathologisation of their condition under therapeutic governance in greater
numbers is testimony to people’s capacity and resilience.
Chapters Seven and
Thirteen revisit the themes of therapeutic governance and social control
where Neville reverses the above framing – where the locus of governance and
control for re-constituting collapsed society is with the marginalized fringe
acting in mutual help. Neville’s process entailed relational governance.
SUMMARY
This chapter has provided a brief background to my
research on therapeutic communities and community mental health in